Heart surgery is the primary method for correcting congenital heart defects in newborns. A major risk of heart surgery is damage to specialized tissue of the conduction system, which generates and propagates electrical impulses necessary for the heart to pump blood throughout the body. Even through the trained eye of a surgeon, it is impossible to discriminate this specialized tissue from the surrounding heart muscle during surgery as it lies beneath the heart’s surface.
“Currently, surgeons rely on guidelines developed from anatomical studies to approximate where it is safe to make an incision or place a suture,” said Chao Huang, a Ph.D. candidate in the department of bioengineering. “Serious complications can occur if this specialized tissue is damaged — usually requiring an artificial pacemaker to be implanted.”
In an effort to improve outcomes in these surgeries, Huang is working to develop a microscopic imaging approach that surgeons can use to discriminate between different types of heart tissue in real-time.
“There were several challenges to this project,” Huang said, “including what features, if any, could be used to discriminate this specialized tissue from other cardiac tissue types, and how to image below the surface of the heart in order to visualize these specialized tissues without disrupting the tissue integrity.”
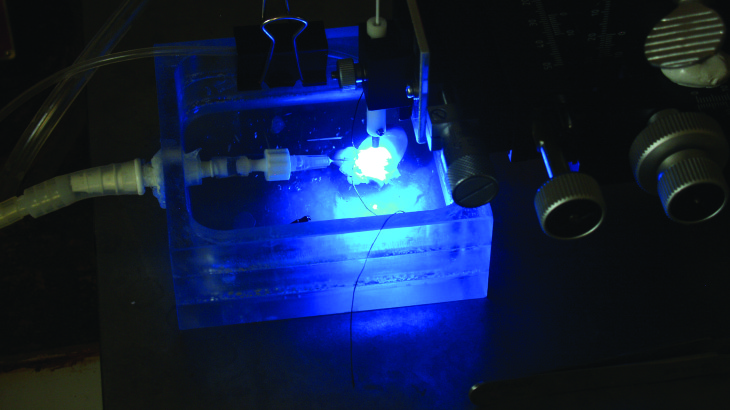
Using an approach based on a recently introduced fiber-optics confocal microscopy system — specialized imaging microprobes and a fluorescent marker of the extracellular space — Huang demonstrated that the specialized tissue of the conduction system could be identified based on its microstructural arrangement. In addition, Huang demonstrated that by configuring the optical properties of the imaging microprobe, images of the specialized tissue could be acquired below the heart surface in a living rat heart.
“We are currently pursuing strategies to further translate our established microscopic imaging approach into the clinical environment,” he said. “In particular, we are exploring FDA-approved fluorescent dyes and development of imaging microprobes specifically for imaging in pediatric hearts.”
By using components that are already FDA-approved, Huang hopes to reduce the number of barriers needed to move the imaging approach into a clinical setting. He believes that the established approach will allow surgeons to reduce the risk of injury to the conduction system during heart surgery and could lead to significant advances in various other surgical disciplines as well.
Huang decided to pursue a Ph.D. in bioengineering after working in industry as an electrical engineer.
“I finally found my passion in life,” he said. “It took going down some tortuous paths, but now I know that my role in life is to develop life-saving technology. I would advise any student not to settle for something they don’t feel 100 percent passionate about.